Delirium
| Delirium | |
|---|---|
| Specialty | Intensive care medicine, Neurology, Psychiatry, Geriatrics |
| Symptoms | Agitation, confusion, drowsiness, hallucinations, delusions, memory problems |
| Usual onset | Any age, but more often in people aged 65 and above |
| Duration | Days to weeks, sometimes months (several hours when caused by anticholinergic medications, like Dicyclomine, Diphenhydramine (Benadryl), Doxylamine, Promethazine) |
| Types | Hyperactive, hypoactive, mixed level of activity |
| Causes | Inconclusive |
| Risk factors | Infection, chronic health problems, certain medications, neurological problems, sleep deprivation, surgery |
| Differential diagnosis | Dementia |
| Treatment | Treating underlying cause, symptomatic management with medication |
| Medication | Depending on the underlying cause |
Delirium (formerly acute confusional state, an ambiguous term which is now discouraged)[1] is a specific state of acute confusion attributable to the direct physiological consequence of a medical condition, effects of a psychoactive substance, or multiple causes, which usually develops over the course of hours to days.[2][3] As a syndrome, delirium presents with disturbances in attention, awareness, and higher-order cognition. People with delirium may experience other neuropsychiatric disturbances including changes in psychomotor activity (e.g., hyperactive, hypoactive, or mixed level of activity), disrupted sleep-wake cycle, emotional disturbances, disturbances of consciousness, or, altered state of consciousness, as well as perceptual disturbances (e.g., hallucinations and delusions), although these features are not required for diagnosis.
Diagnostically, delirium encompasses both the syndrome of acute confusion and its underlying organic process[3] known as an acute encephalopathy.[1] The cause of delirium may be either a disease process inside the brain or a process outside the brain that nonetheless affects the brain. Delirium may be the result of an underlying medical condition (e.g., infection or hypoxia), side effect of a medication such as diphenhydramine, promethazine, and dicyclomine, substance intoxication (e.g., opioids or hallucinogenic deliriants), substance withdrawal (e.g., alcohol or sedatives), or from multiple factors affecting one's overall health (e.g., malnutrition, pain, etc.). In contrast, the emotional and behavioral features due to primary psychiatric disorders (e.g., as in schizophrenia, bipolar disorder) do not meet the diagnostic criteria for 'delirium'.[2]
Delirium may be difficult to diagnose without first establishing a person's usual mental function or 'cognitive baseline'. Delirium can be confused with multiple psychiatric disorders or chronic organic brain syndromes because of many overlapping signs and symptoms in common with dementia, depression, psychosis, etc.[4][5] Delirium may occur in persons with existing mental illness, baseline intellectual disability, or dementia, entirely unrelated to any of these conditions. Delirium is often confused with schizophrenia, psychosis, organic brain syndromes, and more, because of similar signs and symptoms of these disorders.
Treatment of delirium requires identifying and managing the underlying causes, managing delirium symptoms, and reducing the risk of complications.[6] In some cases, temporary or symptomatic treatments are used to comfort the person or to facilitate other care (e.g., preventing people from pulling out a breathing tube). Antipsychotics are not supported for the treatment or prevention of delirium among those who are in hospital; however, they may be used in cases where a person has distressing experiences such as hallucinations or if the person poses a danger to themselves or others.[7][8][9][10][11] When delirium is caused by alcohol or sedative-hypnotic withdrawal, benzodiazepines are typically used as a treatment.[12] There is evidence that the risk of delirium in hospitalized people can be reduced by non-pharmacological care bundles (see Delirium § Prevention).[9] According to the text of DSM-5-TR, although delirium affects only 1–2% of the overall population, 18–35% of adults presenting to the hospital will have delirium, and delirium will occur in 29–65% of people who are hospitalized.[3] Delirium occurs in 11–51% of older adults after surgery, in 81% of those in the ICU, and in 20–22% of individuals in nursing homes or post-acute care settings.[3] Among those requiring critical care, delirium is a risk factor for death within the next year.[3][13]
Because of the confusion caused by similar signs and symptoms of delirium with other neuropsychiatric disorders like schizophrenia and psychosis, treating delirium can be difficult, and might even cause death of the patient due to being treated with the wrong medications.[14][15][16]
Definition
[edit]In common usage, delirium can refer to drowsiness, agitation, disorientation, or hallucinations. In medical terminology, however, the core features of delirium include an acute disturbance in attention, awareness, and global cognition.
Although slight differences exist between the definitions of delirium in the DSM-5-TR[3] and ICD-10,[17] the core features are broadly the same. In 2022, the American Psychiatric Association released the fifth edition text revision of the DSM (DSM-5-TR) with the following criteria for diagnosis:[3]
- A. Disturbance in attention and awareness. This is a required symptom and involves easy distraction, inability to maintain attentional focus, and varying levels of alertness.[18]
- B. Onset is acute (from hours to days), representing a change from baseline mentation and often with fluctuations throughout the day
- C. At least one additional cognitive disturbance (in memory, orientation, language, visuospatial ability, or perception)
- D. The disturbances (criteria A and C) are not better explained by another neurocognitive disorder
- E. There is evidence that the disturbances above are a "direct physiological consequence" of another medical condition, substance intoxication or withdrawal, toxin, or various combinations of causes
Signs and symptoms
[edit]Delirium exists across a range of arousal levels, either as a state between normal wakefulness/alertness and coma (hypoactive) or as a state of heightened psychophysiological arousal (hyperactive). It can also alternate between the two (mixed level of activity). While requiring an acute disturbance in attention, awareness, and cognition, the syndrome of delirium encompasses a broad range of additional neuropsychiatric disturbances.[18]
- Inattention: A disturbance in attention is required for delirium diagnosis. This may present as an impaired ability to direct, focus, sustain, or shift attention.[3]
- Memory impairment: The memory impairment that occurs in delirium is often due to an inability to encode new information, largely as a result of having impaired attention. Older memories already in storage are retained without need of concentration, so previously formed long-term memories (i.e., those formed before the onset of delirium) are usually preserved in all but the most severe cases of delirium, though recall of such information may be impaired due to global impairment in cognition.
- Disorientation: A person may be disoriented to self, place, or time. Additionally, a person may be 'disoriented to situation' and not recognize their environment or appreciate what is going on around them.
- Disorganized thinking: Disorganized thinking is usually noticed with speech that makes limited sense with apparent irrelevancies, and can involve poverty of speech, loose associations, perseveration, tangentiality, and other signs of a formal thought disorder.
- Language disturbances: Anomic aphasia, paraphasia, impaired comprehension, agraphia, and word-finding difficulties all involve impairment of linguistic information processing.
- Sleep/wake disturbances: Sleep disturbances in delirium reflect disruption in both sleep/wake and circadian rhythm regulation, typically characterized by fragmented sleep or even sleep-wake cycle reversal (i.e., active at night, sleeping during the day), including as an early sign preceding the onset of delirium.
- Psychotic and other erroneous beliefs: Symptoms of psychosis include suspiciousness, overvalued ideation and frank delusions. Delusions are typically poorly formed and less stereotyped than in schizophrenia or Alzheimer's disease. They usually relate to persecutory themes of impending danger or threat in the immediate environment (e.g., being poisoned by nurses).
- Perceptual disturbances: These can include illusions, which involve the misperception of real stimuli in the environment, or hallucinations, which involve the perception of stimuli that do not exist.
- Mood lability: Distortions to perceived or communicated emotional states as well as fluctuating emotional states can manifest in delirium (e.g., rapid changes between terror, sadness, joking, fear, anger, and frustration).[19]
- Motor activity changes: Delirium has been commonly classified into psychomotor subtypes of hypoactive, hyperactive, and mixed level of activity,[20] though studies are inconsistent as to their prevalence.[21] Hypoactive cases are prone to non-detection or misdiagnosis as depression. A range of studies suggests that motor subtypes differ regarding underlying pathophysiology, treatment needs, functional prognosis, and risk of mortality, though inconsistent subtype definitions and poorer detection of hypoactive subtypes may influence the interpretation of these findings.[22] The notion of unifying hypoactive and hyperactive states under the construct of delirium is commonly attributed to Lipowski.[23]
- Hyperactive symptoms include hyper-vigilance, restlessness, fast or loud speech, irritability, combativeness, impatience, swearing, singing, laughing, uncooperativeness, euphoria, anger, wandering, easy startling, fast motor responses, distractibility, tangentiality, nightmares, and persistent thoughts (hyperactive sub-typing is defined with at least three of the above).[24]
- Hypoactive symptoms include decreased alertness, sparse or slow speech, lethargy, slowed movements, staring, and apathy.[24]
- Mixed level of activity describes instances of delirium where activity level is either normal or fluctuating between hyperactive and hypoactive.[3]
Causes
[edit]Delirium arises through the interaction of a number of predisposing and precipitating factors.[25][26]
Individuals with multiple and/or significant predisposing factors are at high risk for an episode of delirium with a single and/or mild precipitating factor. Conversely, delirium may only result in low risk individuals if they experience a serious or multiple precipitating factors. These factors can change over time, thus an individual's risk of delirium is modifiable (see Delirium § Prevention).
Predisposing factors
[edit]Important predisposing factors include the following:[26][27]
- 65 or more years of age
- Cognitive impairment/dementia
- Physical morbidity (e.g., biventricular failure, cancer, cerebrovascular disease)
- Psychiatric morbidity (e.g., depression)
- Sensory impairment (i.e., vision and hearing)
- Functional dependence (e.g., requiring assistance for self-care or mobility)
- Dehydration/malnutrition
- Substance use disorder, including alcohol use disorder
Precipitating factors
[edit]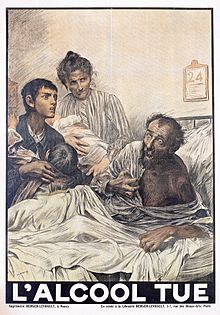
Any serious, acute biological factor that affects neurotransmitter, neuroendocrine, or neuroinflammatory pathways can precipitate an episode of delirium in a vulnerable brain.[28] Certain elements of the clinical environment have also been associated with the risk of developing delirium.[29] Some of the most common precipitating factors are listed below:[26][30]
- Prolonged sleep restriction or deprivation
- Environmental, psychophysiological stress (as found in acute care settings)
- Inadequately controlled pain
- Immobilization, use of physical restraints[31]
- Urinary retention, use of bladder catheter
- Emotional stress
- Severe constipation/fecal impaction
- Medications[32][33]
- Sedatives (benzodiazepines, opioids), anticholinergics, dopaminergics, corticosteroids, polypharmacy
- General anesthetic
- Substance intoxication or withdrawal
- Primary neurologic conditions
- Severe drop in blood pressure, relative to the person's normal blood pressure (orthostatic hypotension) resulting in inadequate blood flow to the brain (cerebral hypoperfusion)
- Stroke/transient ischemic attack(TIA)
- Intracranial bleeding
- Meningitis, encephalitis
- Concurrent illness
- Infections – especially respiratory (e.g. pneumonia, COVID-19[34]) and urinary tract infections
- Iatrogenic complications
- Hypoxia, hypercapnea, anemia
- Poor nutritional status, dehydration, electrolyte imbalances, hypoglycemia
- Shock, heart attacks, heart failure
- Metabolic derangements (e.g. SIADH, Addison's disease, hyperthyroidism)
- Chronic/terminal illness (e.g. cancer)
- Post-traumatic event (e.g. fall, fracture)
- Mercury poisoning (e.g. erethism)
- Major surgery (e.g. cardiac, orthopedic, vascular surgery)
Pathophysiology
[edit]The pathophysiology of delirium is still not well understood, despite extensive research.
Animal models
[edit]The lack of animal models that are relevant to delirium has left many key questions in delirium pathophysiology unanswered. Earliest rodent models of delirium used atropine (a muscarinic acetylcholine receptor blocker) to induce cognitive and electroencephalography (EEG) changes similar to delirium, and other anticholinergic drugs, such as biperiden and hyoscine, have produced similar effects. Along with clinical studies using various drugs with anticholinergic activity, these models have contributed to a "cholinergic deficiency hypothesis" of delirium.[35]
Profound systemic inflammation occurring during sepsis is also known to cause delirium (often termed sepsis-associated encephalopathy).[36] Animal models used to study the interactions between prior degenerative disease and overlying systemic inflammation have shown that even mild systemic inflammation causes acute and transient deficits in working memory among diseased animals.[37] Prior dementia or age-associated cognitive impairment is the primary predisposing factor for clinical delirium and "prior pathology" as defined by these new animal models may consist of synaptic loss, abnormal network connectivity, and "primed microglia" brain macrophages stimulated by prior neurodegenerative disease and aging to amplify subsequent inflammatory responses in the central nervous system (CNS).[37]
Cerebrospinal fluid
[edit]Studies of cerebrospinal fluid (CSF) in delirium are difficult to perform. Apart from the general difficulty of recruiting participants who are often unable to give consent, the inherently invasive nature of CSF sampling makes such research particularly challenging. However, a few studies have managed to sample CSF from persons undergoing spinal anesthesia for elective or emergency surgery.[26][38][39]
A 2018 systematic review showed that, broadly, delirium may be associated with neurotransmitter imbalance (namely serotonin and dopamine signaling), reversible fall in somatostatin, and increased cortisol.[40] The leading "neuroinflammatory hypothesis" (where neurodegenerative disease and aging leads the brain to respond to peripheral inflammation with an exaggerated CNS inflammatory response) has been described,[41] but current evidence is still conflicting and fails to concretely support this hypothesis.[40]
Neuroimaging
[edit]Neuroimaging provides an important avenue to explore the mechanisms that are responsible for delirium.[42][43] Despite progress in the development of magnetic resonance imaging (MRI), the large variety in imaging-based findings has limited our understanding of the changes in the brain that may be linked to delirium. Some challenges associated with imaging people diagnosed with delirium include participant recruitment and inadequate consideration of important confounding factors such as history of dementia and/or depression, which are known to be associated with overlapping changes in the brain also observed on MRI.[42]
Evidence for changes in structural and functional markers include: changes in white-matter integrity (white matter lesions), decreases in brain volume (likely as a result of tissue atrophy), abnormal functional connectivity of brain regions responsible for normal processing of executive function, sensory processing, attention, emotional regulation, memory, and orientation, differences in autoregulation of the vascular vessels in the brain, reduction in cerebral blood flow and possible changes in brain metabolism (including cerebral tissue oxygenation and glucose hypometabolism).[42][43] Altogether, these changes in MRI-based measurements invite further investigation of the mechanisms that may underlie delirium, as a potential avenue to improve clinical management of people with this condition.[42]
Neurophysiology
[edit]Electroencephalography (EEG) allows for continuous capture of global brain function and brain connectivity, and is useful in understanding real-time physiologic changes during delirium.[44] Since the 1950s, delirium has been known to be associated with slowing of resting-state EEG rhythms, with abnormally decreased background alpha power and increased theta and delta frequency activity.[44][45]
From such evidence, a 2018 systematic review proposed a conceptual model that delirium results when insults/stressors trigger a breakdown of brain network dynamics in individuals with low brain resilience (i.e. people who already have underlying problems of low neural connectivity and/or low neuroplasticity like those with Alzheimer's disease).[44]
Neuropathology
[edit]Only a handful of studies exist where there has been an attempt to correlate delirium with pathological findings at autopsy. One research study has been reported on 7 people who died during ICU admission.[46] Each case was admitted with a range of primary pathologies, but all had acute respiratory distress syndrome and/or septic shock contributing to the delirium, 6 showed evidence of low brain perfusion and diffuse vascular injury, and 5 showed hippocampal involvement. A case-control study showed that 9 delirium cases showed higher expression of HLA-DR and CD68 (markers of microglial activation), IL-6 (cytokines pro-inflammatory and anti-inflammatory activities) and GFAP (marker of astrocyte activity) than age-matched controls; this supports a neuroinflammatory cause to delirium, but the conclusions are limited by methodological issues.[47]
A 2017 retrospective study correlating autopsy data with mini–mental state examination (MMSE) scores from 987 brain donors found that delirium combined with a pathological process of dementia accelerated MMSE score decline more than either individual process.[48]
Diagnosis
[edit]The DSM-5-TR criteria are often the standard for diagnosing delirium clinically. However, early recognition of delirium's features using screening instruments, along with taking a careful history, can help in making a diagnosis of delirium. A diagnosis of delirium generally requires knowledge of a person's baseline level of cognitive function. This is especially important for treating people who have neurocognitive or neurodevelopmental disorders, whose baseline mental status may be mistaken as delirium.[49]
General settings
[edit]Guidelines recommend that delirium should be diagnosed consistently when present.[6][50] Much evidence reveals that in most centers delirium is greatly under-diagnosed.[51][52][53][54] A systematic review of large scale routine data studies reporting data on delirium detection tools showed important variations in tool completion rates and tool positive score rates. Some tools, even if completed at high rates, showed delirium positive score rates that there much lower than the expected delirium occurrence level, suggesting low sensitivity in practice.[55]
There is evidence that delirium detection and coding rates can show improvements in response to guidelines and education; for example, whole country data in England and Scotland (sample size 7.7M patients per year) show that there were large increases (3-4 fold) in delirium coding between 2012 and 2020.[56] Delirium detection in general acute care settings can be assisted by the use of validated delirium screening tools. Many such tools have been published, and they differ in a variety of characteristics (e.g., duration, complexity, and need for training). It is also important to ensure that a given tool has been validated for the setting where it is being used.
Examples of tools in use in clinical practice include:
- Confusion Assessment Method (CAM),[57] including variants such as the 3-Minute Diagnostic Interview for the CAM (3D-CAM)[58] and brief CAM (bCAM)[59]
- Delirium Observation Screening Scale (DOS)[60]
- Nursing Delirium Screening Scale (Nu-DESC)[61]
- Recognizing Acute Delirium As part of your Routine (RADAR)[62]
- 4AT (4 A's Test)[63]
- Delirium Diagnostic Tool-Provisional (DDT-Pro),[64][65] also for subsyndromal delirium[66]
Intensive care unit
[edit]People who are in the ICU are at greater risk of delirium, and ICU delirium may lead to prolonged ventilation, longer stays in the hospital, increased stress on family and caregivers, and an increased chance of death.[67] In the ICU, international guidelines recommend that every person admitted gets checked for delirium every day (usually twice or more a day) using a validated clinical tool.[68] Key elements of detecting delirium in the ICU are whether a person can pay attention during a listening task and follow simple commands.[69] The two most widely used are the Confusion Assessment Method for the ICU (CAM-ICU)[70] and the Intensive Care Delirium Screening Checklist (ICDSC).[71] Translations of these tools exist in over 20 languages and are used ICUs globally with instructional videos and implementation tips available.[69] For children in need of intensive care there are validated clinical tools adjusted according to age. The recommended tools are preschool and pediatric Confusion Assessment Methods for the ICU (ps/pCAM-ICU) or the Cornell Assessment for Pediatric Delirium (CAPD) as the most valid and reliable delirium monitoring tools in critically ill children or adolescents.[72]
More emphasis is placed on regular screening over the choice of tool used. This, coupled with proper documentation and informed awareness by the healthcare team, can affect clinical outcomes.[69] Without using one of these tools, 75% of ICU delirium can be missed by the healthcare team, leaving the person without any likely interventions to help reduce the duration of delirium.[69][73]
Differential diagnosis
[edit]There are conditions that might have similar clinical presentations to those seen in delirium. These include dementia,[74][75][76][77][78] depression,[78][76] psychosis,[5][78][76] catatonia,[5] and other conditions that affect cognitive function.[77]
- Dementia: This group of disorders is acquired (non-congenital) with usually irreversible cognitive and psychosocial functional decline. Dementia usually results from an identifiable degenerative brain disease (e.g., Alzheimer disease or Huntington's disease), requires chronic impairment (versus acute onset in delirium), and is typically not associated with changes in level of consciousness.[79] Dementia is different from delirium in that dementia lasts long-term while delirium lasts short-term.
- Depression: Similar symptoms exist between depression and delirium (especially the hypoactive subtype). Gathering a history from other caregivers can clarify baseline mentation.[80]
- Psychosis: In general, people with primary psychosis have intact cognitive function; however, primary psychosis can mimic delirium when it presents with disorganized thoughts and mood dysregulation. This is particularly true in the condition known as delirious mania.[5]
- Other mental illnesses: Some mental illnesses, such as a manic episode of bipolar disorder, depersonalization disorder, or other dissociative conditions, can present with features similar to that of delirium.[5] Such condition, however, would not qualify for a diagnosis of delirium per DSM-5-TR criterion D (i.e., fluctuating cognitive symptoms occurring as part of a primary mental disorder are results of the said mental disorder itself), while physical disorders (e.g., infections, hypoxia, etc.) can precipitate delirium as a mental side-effect/symptom.[3]
Prevention
[edit]Treating delirium that is already established is challenging and for this reason, preventing delirium before it begins is ideal. Prevention approaches include screening to identify people who are at risk, and medication-based and non-medication based (non-pharmacological) treatments.[81]
An estimated 30–40% of all cases of delirium could be prevented in cognitively at-risk populations, and high rates of delirium reflect negatively on the quality of care.[30] Episodes of delirium can be prevented by identifying hospitalized people at risk of the condition. This includes individuals over age 65, with a cognitive impairment, undergoing major surgery, or with severe illness.[50] Routine delirium screening is recommended in such populations. It is thought that a personalized approach to prevention that includes different approaches together can decrease rates of delirium by 27% among the elderly.[82][9]
In 1999, Sharon K. Inouye at Yale University, founded the Hospital Elder Life Program (HELP) [83] which has since become recognized as a proven model for preventing delirium.[84] HELP prevents delirium among the elderly through active participation and engagement with these individuals. There are two working parts to this program, medical professionals such as a trained nurse, and volunteers, who are overseen by the nurse. The volunteer program equips each trainee with the adequate basic geriatric knowledge and interpersonal skills to interact with patients. Volunteers perform the range of motion exercises, cognitive stimulation, and general conversation[85] with elderly patients who are staying in the hospital. Alternative effective delirium prevention programs have been developed, some of which do not require volunteers.[86]
Prevention efforts often fall on caregivers. Caregivers often have a lot expected of them and this is where socioeconomic status plays a role in prevention.[87] If prevention requires constant mental stimulation and daily exercise, this takes time out of the caregiver's day. Based on socioeconomic classes, this may be valuable time that would be used working to support the family. This leads to a disproportionate number of individuals who experience delirium being from marginalized identities.[84] Programs such as the Hospital Elder Life Program can attempt to combat these societal issues by providing additional support and education about delirium that may not otherwise be accessible.
Non-pharmacological
[edit]Delirium may be prevented and treated by using non-pharmacologic approaches focused on risk factors, such as constipation, dehydration, low oxygen levels, immobility, visual or hearing impairment, sleep disturbance, functional decline, and by removing or minimizing problematic medications.[50][76] Ensuring a therapeutic environment (e.g., individualized care, clear communication, adequate reorientation and lighting during daytime, promoting uninterrupted sleep hygiene with minimal noise and light at night, minimizing room relocation, having familiar objects like family pictures, providing earplugs, and providing adequate nutrition, pain control, and assistance toward early mobilization) may also aid in preventing delirium.[9][30][88][89] Research into pharmacologic prevention and treatment is weak and insufficient to make proper recommendations.[76]
Pharmacological
[edit]Melatonin and other pharmacological agents have been studied for delirium prevention, but evidence is conflicting.[9][90] Avoidance or cautious use of benzodiazepines has been recommended for reducing the risk of delirium in critically ill individuals.[91] It is unclear if the medication donepezil, a cholinesterase inhibitor, reduces delirium following surgery.[9] There is also no clear evidence to suggest that citicoline, methylprednisolone, or antipsychotic medications prevent delirium.[9] A review of intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non-cardiac surgery showed little or no difference in postoperative delirium according to the type of anaesthetic maintenance agents[92] in five studies (321 participants). The authors of this review were uncertain whether maintenance of anaesthesia with propofol-based total intravenous anaesthesia (TIVA) or with inhalational agents can affect the incidence rate of postoperative delirium.
Interventions for preventing delirium in long-term care or hospital
The current evidence suggests that software-based interventions to identify medications that could contribute to delirium risk and recommend a pharmacist's medication review probably reduces incidence of delirium in older adults in long-term care.[93] The benefits of hydration reminders and education on risk factors and care homes' solutions for reducing delirium is still uncertain.[93]
For inpatients in a hospital setting, numerous approaches have been suggested to prevent episodes of delirium including targeting risk factors such as sleep deprivation, mobility problems, dehydration, and impairments to a person's sensory system. Often a 'multicomponent' approach by an interdisciplinary team of health care professionals is suggested for people in the hospital at risk of delirium, and there is some evidence that this may decrease to incidence of delirium by up to 43% and may reduce the length of time that the person is hospitalized.[81]
Treatment
[edit]Most often, delirium is reversible; however, people with delirium require treatment for the underlying cause(s) and often to prevent injury and other poor outcomes directly related to delirium.[67]
Treatment of delirium requires attention to multiple domains including the following:[2][30]
- Identify and treat the underlying medical disorder or cause(s)
- Addressing any other possible predisposing and precipitating factors that might be disrupting brain function
- Optimize physiology and conditions for brain recovery (e.g., oxygenation, hydration, nutrition, electrolytes, metabolites, medication review)
- Detect and manage distress and behavioral disturbances (e.g., pain control)
- Maintaining mobility
- Provide rehabilitation through cognitive engagement and mobilization
- Communicate effectively with the person experiencing delirium and their carers or caregivers
- Provide adequate follow-up including consideration of possible dementia and post-traumatic stress.[2]
Multidomain interventions
[edit]These interventions are the first steps in managing acute delirium, and there are many overlaps with delirium preventative strategies.[94] In addition to treating immediate life-threatening causes of delirium (e.g., low O2, low blood pressure, low glucose, dehydration), interventions include optimizing the hospital environment by reducing ambient noise, providing proper lighting, offering pain relief, promoting healthy sleep-wake cycles, and minimizing room changes.[94] Although multicomponent care and comprehensive geriatric care are more specialized for a person experiencing delirium, several studies have been unable to find evidence showing they reduce the duration of delirium.[94]
Family, friends, and other caregivers can offer frequent reassurance, tactile and verbal orientation, cognitive stimulation (e.g. regular visits, familiar objects, clocks, calendars, etc.), and means to stay engaged (e.g. making hearing aids and eyeglasses readily available).[30][50][95] Sometimes verbal and non-verbal deescalation techniques may be required to offer reassurances and calm the person experiencing delirium.[50] Restraints should rarely be used as an intervention for delirium.[96] The use of restraints has been recognized as a risk factor for injury and aggravating symptoms, especially in older hospitalized people with delirium.[96] The only cases where restraints should sparingly be used during delirium is in the protection of life-sustaining interventions, such as endotracheal tubes.[96]
Another approached called the "T-A-DA (tolerate, anticipate, don't agitate) method" can be an effective management technique for older people with delirium, where abnormal behaviors (including hallucinations and delusions) are tolerated and unchallenged, as long as caregiver safety and the safety of the person experiencing delirium is not threatened.[76] Implementation of this model may require a designated area in the hospital. All unnecessary attachments are removed to anticipate for greater mobility, and agitation is prevented by avoiding excessive reorientation/questioning.[76]
Medications
[edit]The use of medications for delirium is generally restricted to managing its distressing or dangerous neuropsychiatric disturbances. Short-term use (one week or less) of low-dose haloperidol is among the more common pharmacological approaches to delirium.[30][50] Evidence for effectiveness of atypical antipsychotics (e.g. risperidone, olanzapine, ziprasidone, and quetiapine) is emerging, with the benefit for fewer side effects[30][97] Use antipsychotic drugs with caution or not at all for people with conditions such as Parkinson's disease or dementia with Lewy bodies.[50] Evidence for the effectiveness of medications (including antipsychotics and benzodiazepines) in treating delirium is weak.[75][67]
Benzodiazepines can cause or worsen delirium, and there is no reliable evidence of efficacy for treating non-anxiety-related delirium.[98] Similarly, people with dementia with Lewy bodies may have significant side effects with antipsychotics, and should either be treated with a none or small doses of benzodiazepines.[50]
The antidepressant trazodone is occasionally used in the treatment of delirium, but it carries a risk of over-sedation, and its use has not been well studied.[30]
For adults with delirium that are in the ICU, medications are used commonly to improve the symptoms. Dexmedetomidine may shorten the length of the delirium in adults who are critically ill, and rivastigmine is not suggested.[67] For adults with delirium who are near the end of their life (on palliative care) high quality evidence to support or refute the use of most medications to treat delirium is not available.[99] Low quality evidence indicates that the antipsychotic medications risperidone or haloperidol may make the delirium slightly worse in people who are terminally ill, when compared to a placebo treatment.[99] There is also moderate to low quality evidence to suggest that haloperidol and risperidone may be associated with a slight increase in side effects, specifically extrapyramidal symptoms, if the person near the end of their life has delirium that is mild to moderate in severity.[99]
Prognosis
[edit]There is substantial evidence that delirium results in long-term poor outcomes in older persons admitted to hospital.[100] This systematic review only included studies that looked for an independent effect of delirium (i.e., after accounting for other associations with poor outcomes, for example co-morbidity or illness severity).
In older persons admitted to hospital, individuals experiencing delirium are twice as likely to die than those who do not (meta-analysis of 12 studies).[100] In the only prospective study conducted in the general population, older persons reporting delirium also showed higher mortality (60% increase).[101] A large (N=82,770) two-centre study in unselected older emergency population found that delirium detected as part of normal care using the 4AT tool was strongly linked to 30-day mortality, hospital length of stay, and days at home in the year following the 4AT test date.[102]
Institutionalization was also twice as likely after an admission with delirium (meta-analysis of seven studies).[100] In a community-based population examining individuals after an episode of severe infection (though not specifically delirium), these persons acquired more functional limitations (i.e., required more assistance with their care needs) than those not experiencing infection.[103] After an episode of delirium in the general population, functional dependence increased threefold.[101]
The association between delirium and dementia is complex. The systematic review estimated a 13-fold increase in dementia after delirium (meta-analysis of two studies).[100] However, it is difficult to be certain that this is accurate because the population admitted to hospital includes persons with undiagnosed dementia (i.e., the dementia was present before the delirium, rather than caused by it). In prospective studies, people hospitalised from any cause appear to be at greater risk of dementia[104] and faster trajectories of cognitive decline,[104][105] but these studies did not specifically look at delirium. In the only population-based prospective study of delirium, older persons had an eight-fold increase in dementia and faster cognitive decline.[101] The same association is also evident in persons already diagnosed with Alzheimer's dementia.[106]
Recent long-term studies showed that many people still meet criteria for delirium for a prolonged period after hospital discharge, with up to 21% of people showing persistent delirium at 6 months post-discharge.[107]
Dementia in ICU survivors
[edit]Between 50% and 70% of people admitted to the ICU have permanent problems with brain dysfunction similar to those experienced by people with Alzheimer's or those with a traumatic brain injury, leaving many ICU survivors permanently disabled.[108] This is a distressing personal and public health problem and continues to receive increasing attention in ongoing investigations.[109][98]
The implications of such an "acquired dementia-like illness" can profoundly debilitate a person's livelihood level, often dismantling his/her life in practical ways like impairing one's ability to find a car in a parking lot, complete shopping lists, or perform job-related tasks done previously for years.[109] The societal implications can be enormous when considering work-force issues related to the inability of wage-earners to work due to their own ICU stay or that of someone else they must care for.[110]
Epidemiology
[edit]The highest rates of delirium (often 50–75% of people) occur among those who are critically ill in the intensive care unit (ICU).[111] This was historically referred to as "ICU psychosis" or "ICU syndrome"; however, these terms are now widely disfavored in relation to the operationalized term ICU delirium. Since the advent of validated and easy-to-implement delirium instruments for people admitted to the ICU such as the Confusion Assessment Method for the ICU (CAM-ICU)[70] and the Intensive Care Delirium Screening Checklist (ICDSC),[71] it has been recognized that most ICU delirium is hypoactive, and can easily be missed unless evaluated regularly. The causes of delirium depend on the underlying illnesses, new problems like sepsis and low oxygen levels, and the sedative and pain medicines that are nearly universally given to all ICU patients. Outside the ICU, on hospital wards and in nursing homes, the problem of delirium is also a very important medical problem, especially for older patients.[112]
The most recent area of the hospital in which delirium is just beginning to be monitored routinely in many centers is the Emergency Department, where the prevalence of delirium among older adults is about 10%.[113] A systematic review of delirium in general medical inpatients showed that estimates of delirium prevalence on admission ranged 10–31%.[114] About 5–10% of older adults who are admitted to hospital develop a new episode of delirium while in hospital.[113] Rates of delirium vary widely across general hospital wards.[115] Estimates of the prevalence of delirium in nursing homes are between 10%[113] and 45%.[116]
Society and culture
[edit]Delirium is one of the oldest forms of mental disorder known in medical history.[117] The Roman author Aulus Cornelius Celsus used the term to describe mental disturbance from head trauma or fever in his work De Medicina.[118] Sims (1995, p. 31) points out a "superb detailed and lengthy description" of delirium in "The Stroller's Tale" from Charles Dickens' The Pickwick Papers.[119][120] Historically, delirium has also been noted for its cognitive sequelae. For instance, the English medical writer Philip Barrow noted in 1583 that if delirium (or "frensy") resolves, it may be followed by a loss of memory and reasoning power.[121]
Costs
[edit]In the US, the cost of a hospital admission for people with delirium is estimated at between $16k and $64k, suggesting the national burden of delirium may range from $38 bn to $150 bn per year (2008 estimate).[122] In the UK, the cost is estimated as £13k per admission.[123]
References
[edit]- ^ a b Slooter AJ, Otte WM, Devlin JW, Arora RC, Bleck TP, Claassen J, et al. (May 2020). "Updated nomenclature of delirium and acute encephalopathy: statement of ten Societies". Intensive Care Medicine. 46 (5): 1020–1022. doi:10.1007/s00134-019-05907-4. PMC 7210231. PMID 32055887.
- ^ a b c d Wilson JE, Mart MF, Cunningham C, Shehabi Y, Girard TD, MacLullich AM, et al. (November 2020). "Delirium". Nature Reviews. Disease Primers. 6 (1): 90. doi:10.1038/s41572-020-00223-4. PMC 9012267. PMID 33184265. S2CID 226302415.
- ^ a b c d e f g h i j "Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR™)". American Psychiatric Association. Archived from the original on April 22, 2022. Retrieved April 18, 2022.
- ^ Gleason OC (March 2003). "Delirium". American Family Physician. 67 (5): 1027–1034. PMID 12643363. Archived from the original on 2011-06-06.
- ^ a b c d e Wilson JE, Andrews P, Ainsworth A, Roy K, Ely EW, Oldham MA (Fall 2021). "Pseudodelirium: Psychiatric Conditions to Consider on the Differential for Delirium". The Journal of Neuropsychiatry and Clinical Neurosciences. 33 (4): 356–364. doi:10.1176/appi.neuropsych.20120316. PMC 8929410. PMID 34392693.
- ^ a b "SIGN 157 Delirium". www.sign.ac.uk. Archived from the original on 2022-12-06. Retrieved 2020-05-15.
- ^ Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJ, Pandharipande PP, et al. (September 2018). "Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU". Critical Care Medicine. 46 (9): e825–e873. doi:10.1097/CCM.0000000000003299. PMID 30113379.
- ^ Santos CD, Rose MQ (June 2021). "Extrapyramidal Symptoms Induced by Treatment for Delirium: A Case Report". Critical Care Nurse. 41 (3): 50–54. doi:10.4037/ccn2021765. PMID 34061189.
- ^ a b c d e f g Siddiqi N, Harrison JK, Clegg A, Teale EA, Young J, Taylor J, et al. (March 2016). "Interventions for preventing delirium in hospitalised non-ICU patients". The Cochrane Database of Systematic Reviews. 2016 (3): CD005563. doi:10.1002/14651858.CD005563.pub3. PMC 10431752. PMID 26967259.
- ^ Neufeld KJ, Yue J, Robinson TN, Inouye SK, Needham DM (April 2016). "Antipsychotic Medication for Prevention and Treatment of Delirium in Hospitalized Adults: A Systematic Review and Meta-Analysis". Journal of the American Geriatrics Society. 64 (4): 705–714. doi:10.1111/jgs.14076. PMC 4840067. PMID 27004732.
- ^ Burry L, Mehta S, Perreault MM, Luxenberg JS, Siddiqi N, Hutton B, et al. (June 2018). "Antipsychotics for treatment of delirium in hospitalised non-ICU patients". The Cochrane Database of Systematic Reviews. 2018 (6): CD005594. doi:10.1002/14651858.CD005594.pub3. PMC 6513380. PMID 29920656. Archived from the original on 2019-11-07. Retrieved 2019-11-07.
- ^ Attard A, Ranjith G, Taylor D (August 2008). "Delirium and its treatment". CNS Drugs. 22 (8): 631–644. doi:10.2165/00023210-200822080-00002. PMID 18601302. S2CID 94743.
- ^ Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE, et al. (April 2004). "Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit". JAMA. 291 (14): 1753–1762. doi:10.1001/jama.291.14.1753. PMID 15082703.
- ^ Dharmarajan K, Swami S, Gou RY, Jones RN, Inouye SK (May 2017). "Pathway from Delirium to Death: Potential In-Hospital Mediators of Excess Mortality". Journal of the American Geriatrics Society. 65 (5): 1026–1033. doi:10.1111/jgs.14743. PMC 5435507. PMID 28039852.
- ^ Rockwood K, Cosway S, Carver D, Jarrett P, Stadnyk K, Fisk J (October 1999). "The risk of dementia and death after delirium". Age and Ageing. 28 (6): 551–556. doi:10.1093/ageing/28.6.551. PMID 10604507.
- ^ Leslie DL, Zhang Y, Holford TR, Bogardus ST, Leo-Summers LS, Inouye SK (July 2005). "Premature death associated with delirium at 1-year follow-up". Archives of Internal Medicine. 165 (14): 1657–1662. doi:10.1001/archinte.165.14.1657. PMID 16043686.
- ^ Sartorius N, Henderson A, Strotzka H, Lipowski Z, Yu-cun S, You-xin X, et al. "The ICD-10 Classification of Mental and Behavioural Disorders Clinical descriptions and diagnostic guidelines" (PDF). www.who.int World Health Organization. Microsoft Word. bluebook.doc. pp. 56–7. Archived (PDF) from the original on 2004-10-17. Retrieved 23 June 2021 – via Microsoft Bing.
- ^ a b Hales RE, Yudofsky SC, Gabbard GO, eds. (2008). The American Psychiatric Publishing textbook of psychiatry (5th ed.). Washington, DC: American Psychiatric Publishing. ISBN 9781585622573. OCLC 145554590.
- ^ Leentjens AF, Rundell J, Rummans T, Shim JJ, Oldham R, Peterson L, et al. (August 2012). "Delirium: An evidence-based medicine (EBM) monograph for psychosomatic medicine practice, commissioned by the Academy of Psychosomatic Medicine (APM) and the European Association of Consultation Liaison Psychiatry and Psychosomatics (EACLPP)". Journal of Psychosomatic Research. 73 (2): 149–152. doi:10.1016/j.jpsychores.2012.05.009. PMID 22789420.
- ^ Lipowski ZJ (March 1989). "Delirium in the elderly patient". The New England Journal of Medicine. 320 (9): 578–582. doi:10.1056/NEJM198903023200907. PMID 2644535.
- ^ de Rooij SE, Schuurmans MJ, van der Mast RC, Levi M (July 2005). "Clinical subtypes of delirium and their relevance for daily clinical practice: a systematic review". International Journal of Geriatric Psychiatry. 20 (7): 609–615. doi:10.1002/gps.1343. PMID 16021665. S2CID 37993802.
- ^ Meagher D (February 2009). "Motor subtypes of delirium: past, present and future". International Review of Psychiatry. 21 (1): 59–73. doi:10.1080/09540260802675460. PMID 19219713. S2CID 11705848.
- ^ Delirium: Acute Brian Failure in Man. Springfield, IL: Charles C Thomas. 1980. ISBN 0-398-03909-7.
- ^ a b Liptzin B, Levkoff SE (December 1992). "An empirical study of delirium subtypes". The British Journal of Psychiatry. 161 (6): 843–845. doi:10.1192/bjp.161.6.843. PMID 1483173. S2CID 8754215.
- ^ Magny E, Le Petitcorps H, Pociumban M, Bouksani-Kacher Z, Pautas É, Belmin J, et al. (2018-02-23). "Predisposing and precipitating factors for delirium in community-dwelling older adults admitted to hospital with this condition: A prospective case series". PLOS ONE. 13 (2): e0193034. Bibcode:2018PLoSO..1393034M. doi:10.1371/journal.pone.0193034. PMC 5825033. PMID 29474380.
- ^ a b c d Ormseth CH, LaHue SC, Oldham MA, Josephson SA, Whitaker E, Douglas VC (January 2023). "Predisposing and Precipitating Factors Associated With Delirium: A Systematic Review". JAMA Network Open. 6 (1): e2249950. doi:10.1001/jamanetworkopen.2022.49950. PMC 9856673. PMID 36607634.
- ^ Fong TG, Tulebaev SR, Inouye SK (April 2009). "Delirium in elderly adults: diagnosis, prevention and treatment". Nature Reviews. Neurology. 5 (4): 210–220. doi:10.1038/nrneurol.2009.24. PMC 3065676. PMID 19347026.
- ^ Hughes CG, Patel MB, Pandharipande PP (October 2012). "Pathophysiology of acute brain dysfunction: what's the cause of all this confusion?". Current Opinion in Critical Care. 18 (5): 518–526. doi:10.1097/MCC.0b013e328357effa. PMID 22941208. S2CID 22572990.
- ^ McCusker J, Cole M, Abrahamowicz M, Han L, Podoba JE, Ramman-Haddad L (October 2001). "Environmental risk factors for delirium in hospitalized older people". Journal of the American Geriatrics Society. 49 (10): 1327–1334. doi:10.1046/j.1532-5415.2001.49260.x. PMID 11890491. S2CID 22910426.
- ^ a b c d e f g h Inouye SK (March 2006). "Delirium in older persons". The New England Journal of Medicine. 354 (11): 1157–1165. doi:10.1056/NEJMra052321. PMID 16540616. S2CID 245337. Archived from the original on 2021-08-28. Retrieved 2019-01-04.
- ^ Rollo E, Callea A, Brunetti V, Vollono C, Marotta J, Imperatori C, et al. (May 2021). "Delirium in acute stroke: A prospective, cross-sectional, cohort study". European Journal of Neurology. 28 (5): 1590–1600. doi:10.1111/ene.14749. PMID 33476475. S2CID 231677499.
- ^ Clegg A, Young JB (January 2011). "Which medications to avoid in people at risk of delirium: a systematic review". Age and Ageing. 40 (1): 23–29. doi:10.1093/ageing/afq140. PMID 21068014.
- ^ McCoy TH, Castro VM, Hart KL, Perlis RH (July 2021). "Stratified delirium risk using prescription medication data in a state-wide cohort". General Hospital Psychiatry. 71: 114–120. doi:10.1016/j.genhosppsych.2021.05.001. PMC 8249339. PMID 34091195.
- ^ Saini A, Oh TH, Ghanem DA, Castro M, Butler M, Sin Fai Lam CC, et al. (October 2022). "Inflammatory and blood gas markers of COVID-19 delirium compared to non-COVID-19 delirium: a cross-sectional study". Aging & Mental Health. 26 (10): 2054–2061. doi:10.1080/13607863.2021.1989375. PMID 34651536. S2CID 238990849.
- ^ Hshieh TT, Fong TG, Marcantonio ER, Inouye SK (July 2008). "Cholinergic deficiency hypothesis in delirium: a synthesis of current evidence". The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 63 (7): 764–772. doi:10.1093/gerona/63.7.764. PMC 2917793. PMID 18693233.
- ^ Zampieri FG, Park M, Machado FS, Azevedo LC (2011). "Sepsis-associated encephalopathy: not just delirium". Clinics. 66 (10): 1825–1831. doi:10.1590/S1807-59322011001000024. PMC 3180153. PMID 22012058.
- ^ a b Cunningham C, Maclullich AM (February 2013). "At the extreme end of the psychoneuroimmunological spectrum: delirium as a maladaptive sickness behaviour response". Brain, Behavior, and Immunity. 28: 1–13. doi:10.1016/j.bbi.2012.07.012. PMC 4157329. PMID 22884900.
- ^ Derakhshan P, Imani F, Seyed-Siamdoust SA, Garousi S, Nouri N (January 2020). "Cerebrospinal Fluid and Spinal Anesthesia Parameters in Healthy Individuals versus Opium-addict Patients during Lower Limb Surgery". Addiction & Health. 12 (1): 11–17. doi:10.22122/ahj.v12i1.257. PMC 7291896. PMID 32582410.
- ^ Tigchelaar C, Atmosoerodjo SD, van Faassen M, Wardenaar KJ, De Deyn PP, Schoevers RA, et al. (March 2021). "The Anaesthetic Biobank of Cerebrospinal fluid: a unique repository for neuroscientific biomarker research". Annals of Translational Medicine. 9 (6): 455. doi:10.21037/atm-20-4498. PMC 8039635. PMID 33850852.
- ^ a b Hall RJ, Watne LO, Cunningham E, Zetterberg H, Shenkin SD, Wyller TB, et al. (November 2018). "CSF biomarkers in delirium: a systematic review". International Journal of Geriatric Psychiatry. 33 (11): 1479–1500. doi:10.1002/gps.4720. hdl:20.500.11820/5933392d-bf79-4b57-940f-8a5c51f3b02e. PMID 28585290. S2CID 205842730. Archived from the original on 2021-08-28. Retrieved 2019-07-01.
- ^ Cerejeira J, Firmino H, Vaz-Serra A, Mukaetova-Ladinska EB (June 2010). "The neuroinflammatory hypothesis of delirium". Acta Neuropathologica. 119 (6): 737–754. doi:10.1007/s00401-010-0674-1. hdl:10400.4/806. PMID 20309566. S2CID 206972133.
- ^ a b c d Nitchingham A, Kumar V, Shenkin S, Ferguson KJ, Caplan GA (November 2018). "A systematic review of neuroimaging in delirium: predictors, correlates and consequences". International Journal of Geriatric Psychiatry. 33 (11): 1458–1478. doi:10.1002/gps.4724. PMID 28574155. S2CID 20723293.
- ^ a b Soiza RL, Sharma V, Ferguson K, Shenkin SD, Seymour DG, Maclullich AM (September 2008). "Neuroimaging studies of delirium: a systematic review". Journal of Psychosomatic Research. 65 (3): 239–248. doi:10.1016/j.jpsychores.2008.05.021. PMID 18707946.
- ^ a b c Shafi MM, Santarnecchi E, Fong TG, Jones RN, Marcantonio ER, Pascual-Leone A, et al. (June 2017). "Advancing the Neurophysiological Understanding of Delirium". Journal of the American Geriatrics Society. 65 (6): 1114–1118. doi:10.1111/jgs.14748. PMC 5576199. PMID 28165616.
- ^ Engel GL, Romano J (Fall 2004). "Delirium, a syndrome of cerebral insufficiency. 1959". The Journal of Neuropsychiatry and Clinical Neurosciences. 16 (4): 526–538. doi:10.1176/appi.neuropsych.16.4.526. PMID 15616182.
- ^ Janz DR, Abel TW, Jackson JC, Gunther ML, Heckers S, Ely EW (September 2010). "Brain autopsy findings in intensive care unit patients previously suffering from delirium: a pilot study". Journal of Critical Care. 25 (3): 538.e7–538.12. doi:10.1016/j.jcrc.2010.05.004. PMC 3755870. PMID 20580199.
- ^ Munster BC, Aronica E, Zwinderman AH, Eikelenboom P, Cunningham C, Rooij SE (December 2011). "Neuroinflammation in delirium: a postmortem case-control study". Rejuvenation Research. 14 (6): 615–622. doi:10.1089/rej.2011.1185. PMC 4309948. PMID 21978081.
- ^ Davis DH, Muniz-Terrera G, Keage HA, Stephan BC, Fleming J, Ince PG, et al. (March 2017). "Association of Delirium With Cognitive Decline in Late Life: A Neuropathologic Study of 3 Population-Based Cohort Studies". JAMA Psychiatry. 74 (3): 244–251. doi:10.1001/jamapsychiatry.2016.3423. PMC 6037291. PMID 28114436.
- ^ Morandi A, Grossi E, Lucchi E, Zambon A, Faraci B, Severgnini J, et al. (July 2021). "The 4-DSD: A New Tool to Assess Delirium Superimposed on Moderate to Severe Dementia". Journal of the American Medical Directors Association. 22 (7): 1535–1542.e3. doi:10.1016/j.jamda.2021.02.029. PMID 33823162. S2CID 233173770.
- ^ a b c d e f g h "Delirium: Prevention, diagnosis and management in hospital and long-term care". National Institute for Health and Care Excellence. 28 July 2010. Archived from the original on 2023-06-09. Retrieved 2023-01-31.
- ^ Ibitoye T, So S, Shenkin SD, Anand A, Reed MJ, Vardy ER, et al. (2023-05-15). "Delirium is under-reported in discharge summaries and in hospital administrative systems: a systematic review". Delirium. doi:10.56392/001c.74541.
- ^ Bellelli G, Nobili A, Annoni G, Morandi A, Djade CD, Meagher DJ, et al. (November 2015). "Under-detection of delirium and impact of neurocognitive deficits on in-hospital mortality among acute geriatric and medical wards". European Journal of Internal Medicine. 26 (9): 696–704. doi:10.1016/j.ejim.2015.08.006. PMID 26333532.
- ^ Sepulveda E, Franco JG, Trzepacz PT, Gaviria AM, Meagher DJ, Palma J, et al. (May 2016). "Delirium diagnosis defined by cluster analysis of symptoms versus diagnosis by DSM and ICD criteria: diagnostic accuracy study". BMC Psychiatry. 16: 167. doi:10.1186/s12888-016-0878-6. PMC 4882791. PMID 27229307.
- ^ McCoy TH, Snapper L, Stern TA, Perlis RH (2016). "Underreporting of Delirium in Statewide Claims Data: Implications for Clinical Care and Predictive Modeling". Psychosomatics. 57 (5): 480–488. doi:10.1016/j.psym.2016.06.001. PMID 27480944. S2CID 3300073.
- ^ Penfold RS, Squires C, Angus A, Shenkin SD, Ibitoye T, Tieges Z, et al. (May 2024). "Delirium detection tools show varying completion rates and positive score rates when used at scale in routine practice in general hospital settings: A systematic review". Journal of the American Geriatrics Society. 72 (5): 1508–1524. doi:10.1111/jgs.18751. PMID 38241503.
- ^ Ibitoye T, Jackson TA, Davis D, MacLullich AM (July 2023). "Trends in delirium coding rates in older hospital inpatients in England and Scotland: full population data comprising 7.7M patients per year show substantial increases between 2012 and 2020". Delirium Communications. 2023: 84051. doi:10.56392/001c.84051. PMC 7614999. PMID 37654785.
- ^ Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI (December 1990). "Clarifying confusion: the confusion assessment method. A new method for detection of delirium". Annals of Internal Medicine. 113 (12): 941–948. doi:10.7326/0003-4819-113-12-941. PMID 2240918. S2CID 7740657.
- ^ Marcantonio ER, Ngo LH, O'Connor M, Jones RN, Crane PK, Metzger ED, et al. (October 2014). "3D-CAM: derivation and validation of a 3-minute diagnostic interview for CAM-defined delirium: a cross-sectional diagnostic test study". Annals of Internal Medicine. 161 (8): 554–561. doi:10.7326/M14-0865. PMC 4319978. PMID 25329203.
- ^ Han JH, Wilson A, Vasilevskis EE, Shintani A, Schnelle JF, Dittus RS, et al. (November 2013). "Diagnosing delirium in older emergency department patients: validity and reliability of the delirium triage screen and the brief confusion assessment method". Annals of Emergency Medicine. 62 (5): 457–465. doi:10.1016/j.annemergmed.2013.05.003. PMC 3936572. PMID 23916018.
- ^ Schuurmans MJ, Shortridge-Baggett LM, Duursma SA (2003-01-01). "The Delirium Observation Screening Scale: a screening instrument for delirium". Research and Theory for Nursing Practice. 17 (1): 31–50. doi:10.1891/rtnp.17.1.31.53169. PMID 12751884. S2CID 219203272.
- ^ Gaudreau JD, Gagnon P, Harel F, Tremblay A, Roy MA (April 2005). "Fast, systematic, and continuous delirium assessment in hospitalized patients: the nursing delirium screening scale". Journal of Pain and Symptom Management. 29 (4): 368–375. doi:10.1016/j.jpainsymman.2004.07.009. PMID 15857740.
- ^ Voyer P, Champoux N, Desrosiers J, Landreville P, McCusker J, Monette J, et al. (2015-01-01). "Recognizing acute delirium as part of your routine [RADAR]: a validation study". BMC Nursing. 14: 19. doi:10.1186/s12912-015-0070-1. PMC 4384313. PMID 25844067.
- ^ Tieges Z, Maclullich AM, Anand A, Brookes C, Cassarino M, O'connor M, et al. (May 2021). "Diagnostic accuracy of the 4AT for delirium detection in older adults: systematic review and meta-analysis". Age and Ageing. 50 (3): 733–743. doi:10.1093/ageing/afaa224. PMC 8099016. PMID 33951145.
- ^ Kean J, Trzepacz PT, Murray LL, Abell M, Trexler L (2010). "Initial validation of a brief provisional diagnostic scale for delirium". Brain Injury. 24 (10): 1222–1230. doi:10.3109/02699052.2010.498008. PMID 20645705. S2CID 27856235.
- ^ Franco JG, Ocampo MV, Velásquez-Tirado JD, Zaraza DR, Giraldo AM, Serna PA, et al. (2020). "Validation of the Delirium Diagnostic Tool-Provisional (DDT-Pro) With Medical Inpatients and Comparison With the Confusion Assessment Method Algorithm". The Journal of Neuropsychiatry and Clinical Neurosciences. 32 (3): 213–226. doi:10.1176/appi.neuropsych.18110255. PMID 31662094.
- ^ Franco JG, Trzepacz PT, Sepúlveda E, Ocampo MV, Velásquez-Tirado JD, Zaraza DR, et al. (2020). "Delirium diagnostic tool-provisional (DDT-Pro) scores in delirium, subsyndromal delirium and no delirium". General Hospital Psychiatry. 67: 107–114. doi:10.1016/j.genhosppsych.2020.10.003. PMID 33091783. S2CID 225053525.
- ^ a b c d Burry L, Hutton B, Williamson DR, Mehta S, Adhikari NK, Cheng W, et al. (September 2019). "Pharmacological interventions for the treatment of delirium in critically ill adults". The Cochrane Database of Systematic Reviews. 2019 (9): CD011749. doi:10.1002/14651858.CD011749.pub2. PMC 6719921. PMID 31479532.
- ^ Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, et al. (January 2002). "Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult". Critical Care Medicine. 30 (1): 119–141. doi:10.1097/00003246-200201000-00020. PMID 11902253. S2CID 16654002.
- ^ a b c d "Critical Illness, Brain Dysfunction, and Survivorshpi (CIBS) Center". www.icudelirium.org. Archived from the original on 2019-03-22. Retrieved 2019-03-22.
- ^ a b Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, et al. (December 2001). "Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU)". JAMA. 286 (21): 2703–2710. doi:10.1001/jama.286.21.2703. hdl:10818/12438. PMID 11730446.
- ^ a b Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y (May 2001). "Intensive Care Delirium Screening Checklist: evaluation of a new screening tool". Intensive Care Medicine. 27 (5): 859–864. doi:10.1007/s001340100909. PMID 11430542. S2CID 24997942.
- ^ Smith HA, Besunder JB, Betters KA, Johnson PN, Srinivasan V, Stormorken A, et al. (February 2022). "2022 Society of Critical Care Medicine Clinical Practice Guidelines on Prevention and Management of Pain, Agitation, Neuromuscular Blockade, and Delirium in Critically Ill Pediatric Patients With Consideration of the ICU Environment and Early Mobility". Pediatric Critical Care Medicine. 23 (2): e74–e110. doi:10.1097/PCC.0000000000002873. PMID 35119438. S2CID 246530757.
- ^ Jones SF, Pisani MA (April 2012). "ICU delirium: an update". Current Opinion in Critical Care. 18 (2): 146–151. doi:10.1097/MCC.0b013e32835132b9. PMID 22322260. S2CID 404583.
- ^ Wong N, Abraham G. "Treating Delirium & Agitation in the Emergency Room, 2015". EB Medicine. Archived from the original on 2019-12-23. Retrieved 2019-11-25.
- ^ a b Soiza RL, Myint PK (August 2019). "The Scottish Intercollegiate Guidelines Network (SIGN) 157: Guidelines on Risk Reduction and Management of Delirium". Medicina. 55 (8): 491. doi:10.3390/medicina55080491. PMC 6722546. PMID 31443314.
- ^ a b c d e f g Oh ES, Fong TG, Hshieh TT, Inouye SK (September 2017). "Delirium in Older Persons: Advances in Diagnosis and Treatment". JAMA. 318 (12): 1161–1174. doi:10.1001/jama.2017.12067. PMC 5717753. PMID 28973626.
- ^ a b Sugalski G, Ullo M, Winograd SM (February 2019). "Making Sense of Delirium in the Emergency Department". Emergency Medicine Reports. 40 (3). ProQuest 2175238208.
- ^ a b c Grover S, Avasthi A (February 2018). "Clinical Practice Guidelines for Management of Delirium in Elderly". Indian Journal of Psychiatry. 60 (Suppl 3): S329–S340. doi:10.4103/0019-5545.224473. PMC 5840908. PMID 29535468.
- ^ Mendez MF, Cummings JL (2003). Dementia: A Clinical Approach. Butterworth-Heinemann. ISBN 978-0-7506-7470-6. Archived from the original on 2023-12-30. Retrieved 2022-05-17.
- ^ O'Sullivan R, Inouye SK, Meagher D (September 2014). "Delirium and depression: inter-relationship and clinical overlap in elderly people". The Lancet. Psychiatry. 1 (4): 303–311. doi:10.1016/S2215-0366(14)70281-0. PMC 5338740. PMID 26360863.
- ^ a b Burton JK, Craig L, Yong SQ, Siddiqi N, Teale EA, Woodhouse R, et al. (November 2021). "Non-pharmacological interventions for preventing delirium in hospitalised non-ICU patients". The Cochrane Database of Systematic Reviews. 2021 (11): CD013307. doi:10.1002/14651858.CD013307.pub3. PMC 8623130. PMID 34826144.
- ^ Martinez F, Tobar C, Hill N (March 2015). "Preventing delirium: should non-pharmacological, multicomponent interventions be used? A systematic review and meta-analysis of the literature". Age and Ageing. 44 (2): 196–204. doi:10.1093/ageing/afu173. PMID 25424450.
- ^ Hshieh TT, Yang T, Gartaganis SL, Yue J, Inouye SK (October 2018). "Hospital Elder Life Program: Systematic Review and Meta-analysis of Effectiveness". The American Journal of Geriatric Psychiatry. 26 (10): 1015–1033. doi:10.1016/j.jagp.2018.06.007. PMC 6362826. PMID 30076080.
- ^ a b Waite LJ (2004). "The Demographic Faces of the Elderly". Population and Development Review. 30 (Supplement): 3–16. PMC 2614322. PMID 19129925.
- ^ Zachary W, Kirupananthan A, Cotter S, Barbara GH, Cooke RC, Sipho M (2020). "The impact of Hospital Elder Life Program interventions, on 30-day readmission Rates of older hospitalized patients". Archives of Gerontology and Geriatrics. 86: 103963. doi:10.1016/j.archger.2019.103963. PMID 31733512. S2CID 208086667.
- ^ Ludolph P, Stoffers-Winterling J, Kunzler AM, Rösch R, Geschke K, Vahl CF, et al. (August 2020). "Non-Pharmacologic Multicomponent Interventions Preventing Delirium in Hospitalized People". Journal of the American Geriatrics Society. 68 (8): 1864–1871. doi:10.1111/jgs.16565. PMID 32531089.
- ^ Tough H, Brinkhof MW, Siegrist J, Fekete C (December 2019). "Social inequalities in the burden of care: a dyadic analysis in the caregiving partners of persons with a physical disability". International Journal for Equity in Health. 19 (1): 3. doi:10.1186/s12939-019-1112-1. PMC 6938621. PMID 31892324.
- ^ Poongkunran C, John SG, Kannan AS, Shetty S, Bime C, Parthasarathy S (October 2015). "A meta-analysis of sleep-promoting interventions during critical illness". The American Journal of Medicine. 128 (10): 1126–1137.e1. doi:10.1016/j.amjmed.2015.05.026. PMC 4577445. PMID 26071825.
- ^ Flannery AH, Oyler DR, Weinhouse GL (December 2016). "The Impact of Interventions to Improve Sleep on Delirium in the ICU: A Systematic Review and Research Framework". Critical Care Medicine. 44 (12): 2231–2240. doi:10.1097/CCM.0000000000001952. PMID 27509391. S2CID 24494855.
- ^ Gosch M, Nicholas JA (February 2014). "Pharmacologic prevention of postoperative delirium". Zeitschrift für Gerontologie und Geriatrie. 47 (2): 105–109. doi:10.1007/s00391-013-0598-1. PMID 24619041. S2CID 19868320.
- ^ Slooter AJ, Van De Leur RR, Zaal IJ (2017). "Delirium in critically ill patients". Critical Care Neurology Part II. Handbook of Clinical Neurology. Vol. 141. pp. 449–466. doi:10.1016/B978-0-444-63599-0.00025-9. ISBN 9780444635990. PMID 28190430.
- ^ Miller D, Lewis SR, Pritchard MW, Schofield-Robinson OJ, Shelton CL, Alderson P, et al. (August 2018). "Intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non-cardiac surgery". The Cochrane Database of Systematic Reviews. 8 (8): CD012317. doi:10.1002/14651858.CD012317.pub2. PMC 6513211. PMID 30129968.
- ^ a b Woodhouse R, Burton JK, Rana N, Pang YL, Lister JE, Siddiqi N (April 2019). "Interventions for preventing delirium in older people in institutional long-term care". The Cochrane Database of Systematic Reviews. 4 (4): CD009537. doi:10.1002/14651858.cd009537.pub3. PMC 6478111. PMID 31012953.
- ^ a b c Risk reduction and management of delirium: a national clinical guideline. Edinburgh: Scottish Intercollegiate Guidelines Network. 2019. ISBN 978-1-909103-68-9. OCLC 1099827664.
- ^ Rudolph JL, Marcantonio ER (May 2011). "Review articles: postoperative delirium: acute change with long-term implications". Anesthesia and Analgesia. 112 (5): 1202–1211. doi:10.1213/ANE.0b013e3182147f6d. PMC 3090222. PMID 21474660.
- ^ a b c DeWitt MA, Tune LE (2018-07-06), "Delirium", The American Psychiatric Association Publishing Textbook of Neuropsychiatry and Clinical Neurosciences, American Psychiatric Association Publishing, doi:10.1176/appi.books.9781615372423.sy08, ISBN 978-1-61537-187-7, S2CID 240363328
- ^ Tyrer PJ, Silk KR (2008). Cambridge Textbook of Effective Treatments in Psychiatry. Leiden: Cambridge University Press. ISBN 9780511393020. OCLC 437204638.
- ^ a b Roberson SW, Patel MB, Dabrowski W, Ely EW, Pakulski C, Kotfis K (2021-09-14). "Challenges of Delirium Management in Patients with Traumatic Brain Injury: From Pathophysiology to Clinical Practice". Current Neuropharmacology. 19 (9): 1519–1544. doi:10.2174/1570159X19666210119153839. PMC 8762177. PMID 33463474.
- ^ a b c Finucane AM, Jones L, Leurent B, Sampson EL, Stone P, Tookman A, et al. (January 2020). "Drug therapy for delirium in terminally ill adults". The Cochrane Database of Systematic Reviews. 1 (1): CD004770. doi:10.1002/14651858.CD004770.pub3. PMC 6984445. PMID 31960954.
- ^ a b c d Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA (July 2010). "Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis". JAMA. 304 (4): 443–451. doi:10.1001/jama.2010.1013. PMID 20664045. S2CID 13402729.
- ^ a b c Davis DH, Muniz Terrera G, Keage H, Rahkonen T, Oinas M, Matthews FE, et al. (September 2012). "Delirium is a strong risk factor for dementia in the oldest-old: a population-based cohort study". Brain. 135 (Pt 9): 2809–2816. doi:10.1093/brain/aws190. PMC 3437024. PMID 22879644.
- ^ Anand A, Cheng M, Ibitoye T, Maclullich AM, Vardy ER (March 2022). "Positive scores on the 4AT delirium assessment tool at hospital admission are linked to mortality, length of stay and home time: two-centre study of 82,770 emergency admissions". Age and Ageing. 51 (3): afac051. doi:10.1093/ageing/afac051. PMC 8923813. PMID 35292792.
- ^ Iwashyna TJ, Ely EW, Smith DM, Langa KM (October 2010). "Long-term cognitive impairment and functional disability among survivors of severe sepsis". JAMA. 304 (16): 1787–1794. doi:10.1001/jama.2010.1553. PMC 3345288. PMID 20978258.
- ^ a b Ehlenbach WJ, Hough CL, Crane PK, Haneuse SJ, Carson SS, Curtis JR, et al. (February 2010). "Association between acute care and critical illness hospitalization and cognitive function in older adults". JAMA. 303 (8): 763–770. doi:10.1001/jama.2010.167. PMC 2943865. PMID 20179286.
- ^ Wilson RS, Hebert LE, Scherr PA, Dong X, Leurgens SE, Evans DA (March 2012). "Cognitive decline after hospitalization in a community population of older persons". Neurology. 78 (13): 950–956. doi:10.1212/WNL.0b013e31824d5894. PMC 3310309. PMID 22442434.
- ^ Fong TG, Jones RN, Shi P, Marcantonio ER, Yap L, Rudolph JL, et al. (May 2009). "Delirium accelerates cognitive decline in Alzheimer disease". Neurology. 72 (18): 1570–1575. doi:10.1212/WNL.0b013e3181a4129a. PMC 2677515. PMID 19414723.
- ^ Cole MG, Ciampi A, Belzile E, Zhong L (January 2009). "Persistent delirium in older hospital patients: a systematic review of frequency and prognosis". Age and Ageing. 38 (1): 19–26. doi:10.1093/ageing/afn253. PMID 19017678.
- ^ Hopkins RO, Jackson JC (September 2006). "Long-term neurocognitive function after critical illness". Chest. 130 (3): 869–878. doi:10.1378/chest.130.3.869. PMID 16963688. S2CID 8118025.
- ^ a b Harris R (October 10, 2018). "When ICU Delirium Leads To Symptoms Of Dementia After Discharge". NPR. Retrieved January 24, 2024.
- ^ Harris R (October 10, 2018). "When ICU Delirium Leads To Symptoms Of Dementia After Discharge". National Public Radio. Archived from the original on 4 May 2019. Retrieved 29 April 2019.
- ^ Ely EW, et al. "ICU Delirium and Cognitive Impairment Study Group". Vanderbilt University Medical Center. Archived from the original on 10 October 2013. Retrieved 6 December 2012.
- ^ Ryan DJ, O'Regan NA, Caoimh RÓ, Clare J, O'Connor M, Leonard M, et al. (January 2013). "Delirium in an adult acute hospital population: predictors, prevalence and detection". BMJ Open. 3 (1): e001772. doi:10.1136/bmjopen-2012-001772. PMC 3549230. PMID 23299110.
- ^ a b c Canadian Coalition for Seniors' Mental Health (2006). National Guidelines for Seniors' Mental Health: The Assessment and Treatment of Delirium. Canadian Coalition for Seniors' Mental Health. Archived from the original on 2014-09-08.
- ^ Siddiqi N, House AO, Holmes JD (July 2006). "Occurrence and outcome of delirium in medical in-patients: a systematic literature review". Age and Ageing. 35 (4): 350–364. doi:10.1093/ageing/afl005. PMID 16648149.
- ^ McCoy TH, Hart KL, Perlis RH (May 2017). "Characterizing and predicting rates of delirium across general hospital settings". General Hospital Psychiatry. 46: 1–6. doi:10.1016/j.genhosppsych.2017.01.006. PMID 28622808.
- ^ Voyer P, Richard S, Doucet L, Carmichael PH (March 2009). "Detecting delirium and subsyndromal delirium using different diagnostic criteria among demented long-term care residents". Journal of the American Medical Directors Association. 10 (3): 181–188. doi:10.1016/j.jamda.2008.09.006. PMID 19233058.
- ^ Berrios GE (November 1981). "Delirium and confusion in the 19th century: a conceptual history". The British Journal of Psychiatry. 139 (5): 439–449. doi:10.1192/bjp.139.5.439. PMID 7037094. S2CID 145585758.
- ^ Adamis D, Treloar A, Martin FC, Macdonald AJ (December 2007). "A brief review of the history of delirium as a mental disorder". History of Psychiatry. 18 (72 Pt 4): 459–469. doi:10.1177/0957154X07076467. PMID 18590023. S2CID 24424207. Archived from the original on 2019-07-05. Retrieved 2019-07-09.
- ^ Sims A (2002). Symptoms in the mind: an introduction to descriptive psychopathology. Philadelphia: W. B. Saunders. ISBN 978-0-7020-2627-0.
- ^ Dickens C (1837) The Pickwick Papers. Available for free on Project Gutenberg.
- ^ Barrough P (1583). The methode of phisicke conteyning the causes, signes, and cures of invvard diseases in mans body from the head to the foote. VVhereunto is added, the forme and rule of making remedies and medicines, which our phisitians commonly vse at this day, with the proportion, quantitie, & names of ech [sic] medicine. London: By Thomas Vautroullier dwelling in the Blacke-friars by Lud-gate. p. 18. Archived from the original on 2020-07-30. Retrieved 2020-04-23.
- ^ Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK (January 2008). "One-year health care costs associated with delirium in the elderly population". Archives of Internal Medicine. 168 (1): 27–32. doi:10.1001/archinternmed.2007.4. PMC 4559525. PMID 18195192.
- ^ Akunne A, Murthy L, Young J (May 2012). "Cost-effectiveness of multi-component interventions to prevent delirium in older people admitted to medical wards". Age and Ageing. 41 (3): 285–291. doi:10.1093/ageing/afr147. PMID 22282171.
Further reading
[edit]- Macdonald A, Lindesay J, Rockwood K (2002). Delirium in old age. Oxford [Oxfordshire]: Oxford University Press. ISBN 978-0-19-263275-3.
- Grassi L, Caraceni A (2003). Delirium: acute confusional states in palliative medicine. Oxford: Oxford University Press. ISBN 978-0192631992.
- Newman JK, Slater CT, eds. (2012). Delirium: causes, diagnosis and treatment. Hauppauge, N.Y.: Nova Science Publisher's, Inc. ISBN 978-1613242940.
